 Photo by Polina Zimmerman
Photo by Polina ZimmermanOriginally Posted On: https://www.azgyn.com/blog/what-is-endometriosis/
Endometriosis is a uterine condition that affects as many as 1 in every 10 women during their childbearing years, or about 175 million women worldwide. Women with endometriosis experience a wide range of symptoms, and it’s crucial to understand this condition’s effects on a woman’s body and identify its existence as soon as possible.
Left unchecked, endometriosis can cause chronic, daily, and even debilitating pain for women and girls who experience it. Prolonged, unidentified endometriosis can even cause infertility; in fact, about 30 to 40 percent of women with endometriosis will experience infertility because of the condition. In addition, some of the symptoms of endometriosis can masquerade as other, common uterine and hormone-related conditions, lengthening the time to diagnosis and increasing infertility risks.
For that reason, early identification and treatment is crucial. Some women with endometriosis can manage the symptoms with simple treatments like hormone therapy or birth control, while others may require surgery. Building a wealth of knowledge about the condition can help you identify it, seek treatment, and make more informed decisions regarding the treatment process.
How Does Endometriosis Occur?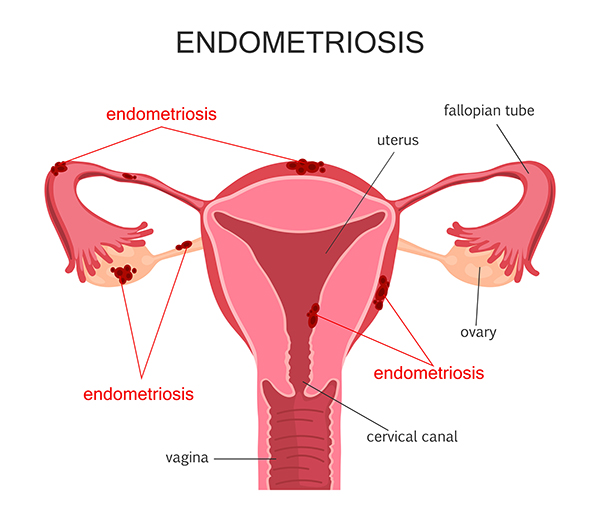
As you may have suspected, endometriosis involves the uterus as well as potentially other reproductive organs within the woman’s body. The endometrium is the tissue that lines the walls of the uterus, and endometriosis is a condition that affects these tissues. During a normal menstrual cycle, the endometrium builds up in anticipation of pregnancy, where it is needed to help sustain a growing embryo or fetus; when pregnancy does not occur, the endometrium breaks down and is shed via menstruation.
A woman with endometriosis will start accumulating endometrial tissue outside the uterus, usually inside the abdominal cavity. Unfortunately, the tissues outside the uterus still respond to the menstrual cycle the same as the tissues inside the uterus. Once a period begins, these tissues will break apart and bleed. While the endometrium tissues inside the uterus can exit through the cervix, the tissues outside the uterus have nowhere to go.
How Does Endometriosis Affect Women?The endometrium tissues that dissolve and bleed in the abdominal cavity will aggravate the other tissues around the uterus and cause inflammation, swelling and severe cramping pains. Doctors refer to the tissues scarred by endometrial tissues as nodules, implants, growths or lesions. This scarred, misplaced tissue is what causes the pain or discomfort common to endometriosis and can lead to the infertility so common to the condition. However, the exact symptoms experienced often depend on the location of the endometrium outside the uterus.
Most commonly, endometriosis affects:
- Ovaries
- Fallopian tubes
- Ligaments supporting the uterus
- The area between the uterus and the rectum
- The outside of the uterus
- The lining of the pelvic cavity
In rare cases, endometrium tissues can accumulate in the intestines, anus, bladder, cervix, vagina or vulva, including previous abdominal surgery scars. In extremely rare cases, doctors have located endometrial tissues in patients’ thighs, arms and lungs.
Endometriosis is a progressive condition that may not manifest noticeable symptoms until many years after menstrual periods begin. Each cycle causes more endometrium accumulation. Over the years, the endometrium implants grow and affect more tissues. Menopause generally causes the symptoms of endometriosis to subside and the implants to deteriorate.
What Causes Endometriosis?While researchers have made many discoveries regarding what happens to the tissues affected by endometriosis, the exact endometriosis causes remain unknown. Currently, the only endometriosis cases that can be linked to a definitive cause are those where direct transplantation – the transferal of endometrial tissue onto the abdominal wall after a caesarean section or other uterine surgery – has occurred.
Popular, evidence-based theories include:
- Travel theories, in which researchers posit that endometrial tissues may travel via the blood and lymphatic systems and implant elsewhere in the body.
- Reverse menstruation, in which some menstrual tissue reverses direction within the fallopian tubes and into the abdomen, where it implants.
- Transformation, in which researchers suggest that other types of cells in any location may transform spontaneously into endometrial cells.
While research is ongoing, in an attempt to determine the root cause of endometriosis, researchers agree there may be a genetic component as well. Some women, due to genetic family history, may be predisposed to endometriosis.
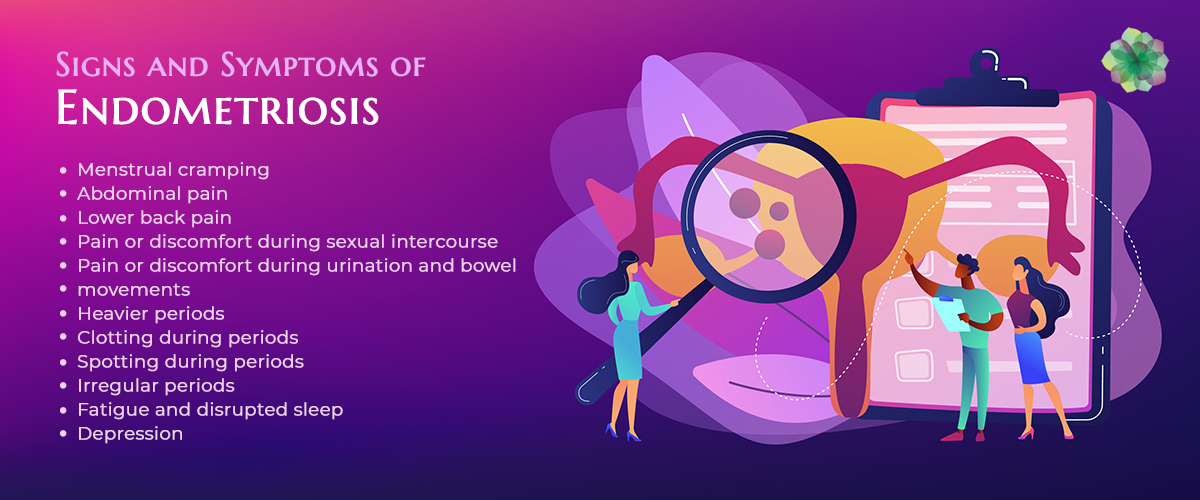
As mentioned earlier, identifying endometriosis symptoms early can allow for earlier treatment of the condition, perhaps reducing the chances women will experience infertility as a result. The early symptoms of endometriosis typically include more significant:
- Menstrual cramping
- Abdominal pain
- Lower back pain
- Pain or discomfort during sexual intercourse
- Pain or discomfort during urination and bowel movements
- Heavier periods
- Clotting during periods
- Spotting during periods
- Irregular periods
- Fatigue and disrupted sleep
- Depression
If endometriosis is allowed to progress, symptoms can spread beyond the reproductive system itself and into the other abdominal systems it affects. Endometrium implants can cause irritation that can progress into infections, abscesses or areas of the body that are tender to the touch. If endometriosis affects the tissues of the intestines or bladder, it can cause urinary or intestinal pains as well.
Endometriosis and PCOS FertilityAlthough endometriosis is a fairly well-known and well-documented condition that causes infertility, it’s often confused with another common reproductive disorder known as polycystic ovary syndrome, or PCOS. Both conditions can cause infertility but distinguishing between the two is important, since treatment regimens differ. So, what is PCOS and how is it different?
Simply put, while endometriosis involves the transferal and growth of the endometrium outside of the uterus, PCOS involves the ovaries. With PCOS, the ovaries don’t ovulate as they should, causing egg follicles to become stuck inside. While, on the surface, endometriosis and PCOS can feel like depression, “period pain” or “abdominal pain”, their primary symptoms and the method of diagnosis differ greatly.
Diagnosing Endometriosis CasesA doctor will need to review a patient’s entire gynecological history to properly diagnose endometriosis. The doctor must also perform a full physical examination and a pelvic examination. In some cases where doctors have reason to believe endometrial tissue may have spread to other, specific areas within the pelvis, doctors may perform an ultrasound, CT scan or MRI to provide images of the organs in question.
However, a positive diagnosis is only confirmed with a laparoscopic procedure. During this procedure, the patient is typically subject to general anesthesia, and the abdomen inflated with air via a small needle; this allows the doctor to have a better view of all components of the abdominal cavity. Then, the doctor will insert a lighted laparoscopic surgical instrument through a small abdominal incision to view the internal organs and locate endometrial implants. Overall, the procedure takes approximately 30 to 45 minutes.
Based on the findings during the laparoscopy, the doctor will be able to confirm the presence of endometriosis. However, doctors rarely eliminate the possibility of endometriosis, since endometrial growths may be tiny, or hidden by other tissues. Next, the doctor will rate the severity of the endometriosis present.
Determining Endometriosis SeverityThe American Society of Reproductive Medicine has established a classification system for endometriosis, which is as follows:
- Stage 1 – Minimal presence of endometriosis
- Stage 2 – Mild presence of endometriosis
- Stage 3 – Moderate presence of endometriosis
- Stage 4 – Severe presence of endometriosis
To determine which stage each case of endometriosis falls under, doctors must first consider a number of factors, including:
- The amount of tissue accumulation
- The location of those tissues
- The amount of scar tissue involved
- The spread of the scar tissue within the abdominal cavity
- Whether pelvic structures like the pelvic cavity or the pelvic floor are involved
- Fallopian tube blockage
- The presence of pelvic adhesions
- The severity of the patient’s symptoms
Small, isolated endometrial implants are usually considered mild endometriosis, while more significant lesions would be moderate to severe endometriosis. More severe cases of endometriosis will also create more scar tissue, potentially involving the structural components of the pelvis, causing blockage of the Fallopian tubes and other organs.
Treatment Options for EndometriosisWomen diagnosed with endometriosis have a number of treatment options available, based on many factors such as overall health, the severity of the condition, tolerance for certain treatments, and the expected outcome of treatment. Endometriosis treatment may include:
- Rest and relaxation. Avoiding stress, heat therapy, taking warm baths, and other relaxation techniques can help relieve minor symptoms of endometriosis and dyspareunia.
- Diet changes. For minor cases, doctors may suggest a diet for endometriosis and fertility. Typically, this includes avoiding caffeine, alcohol, red meat and processed foods, as well as increasing consumption of fruits, vegetables, Omega 3s and soy.
- OTC medications. Doctors suggest simple pain medications such as ibuprofen for mild cases of endometriosis or other over the counter treatments like CBD endometriosis pain relievers.
- Hormone therapy. Hormone treatment is very effective for small, isolated endometrial implants. Oral contraceptives that contain estrogen and progestin or synthetic progestin pills can provide relief in some cases.
- Hormone blocking. Other women may require more robust treatments with synthetic pituitary blockers or gonadotropin-releasing hormone agonists. These medications block hormones from the pituitary gland that contribute to the menstrual cycle. While these monthly injections are effective for some women, they also cause bone mineral loss.
For women who want to become pregnant after treatment of endometriosis, the first three options are often considered the most conducive to a healthy pregnancy in the future. Some women opt for temporary hormone suppression therapy, so they can attempt to conceive afterward. For other patients, hormone suppressants can be an effective solution with the added benefit of preventing pregnancy, if desired. Still others require surgery to treat the cause of endometriosis pain.
Surgical OptionsSome women with severe endometriosis will require surgery for relief. In these cases, surgeons will try to remove as much of the endometrium implants as possible without risking damage to the surrounding tissues. Primarily, endometriosis surgery is limited to three distinct options:
- Laparoscopy. Some surgeons opt for laparoscopic laser removal, which begins with the same process used to diagnose endometriosis. Once endometrial tissue is found, the surgeon will cauterize and vaporize sections of endometrial tissue. Laparoscopic procedures are minimally invasive and have shorter recovery times than typical abdominal surgeries.
- Laparotomy. For advanced cases, more drastic surgical options may be the only solution. A laparotomy uses a much larger incision into the abdominal cavity to expose more of the interior to the surgeon. Then, a similar procedure is used to excise the endometrial tissue. With a larger incision comes a more extended recovery period post-surgery.
- Hysterectomy. For the most severe or advanced cases, a hysterectomy may be required to stop the symptoms of endometriosis. During this procedure, a surgeon removes the uterus altogether, either laparoscopically, through a large incision, or even through the vagina. In some cases, the ovaries are removed as well to inhibit tissue growth. After hysterectomy, future pregnancy is not possible.
While conservative surgery is a safe and effective way to treat endometriosis, it’s important to treat as early as possible. In fact, as many as 40% of advanced endometriosis patients experience symptoms within five years as the result of tissue regrowth. More drastic surgeries such as hysterectomy with ovary removal do a better job of eliminating existing tissue and the hormone swings that cause it to grow, but regrowth and infertility is still possible. Thus, it’s vital for any woman considering any level of surgery to discuss the issue at length with her doctor.
Take Control of Your Uterine Health with Endometriosis Specialists in ArizonaKeeping close tabs on your menstrual cycles and uterine health are important at any age. Every endometriosis case is different, but your case can be manageable with early detection, symptom management and careful screening. The providers who work with Arizona Gynecology Consultants can handle any aspect of gynecological care, so contact us today if you would like more information about endometriosis or treatment options.

